Mpox in Ontario: ‘It’s crucial to get a second dose,’ U of T expert says
July 29/2024
Rising mpox cases and a new variant of the virus are renewing calls for vaccination.
By: Ishani Nath
This post was originally published on July 29 and has been updated to include Daniel Grace and more recent mpox data on November 4.
Mpox is raising renewed calls for vaccination across Canada and around the world.
With a new form of the virus circulating, and an increased number of cases particularly in Africa, the World Health Organization again declared mpox a public health emergency of international concern in August. In Canada, there have been 315 confirmed cases so far this year.
Mpox, which was previously referred to as monkeypox, is a viral illness that can cause a skin rash along with flu-like systems like fever, body aches and low energy. While many recover from mpox, some individuals can become seriously ill and die from the disease.
“We’re seeing more cases now compared to last year so it’s important to remind those eligible to get vaccinated and stay protected against this virus,” says Ramandip Grewal, an Assistant Professor at the Centre for Vaccine Preventable Diseases (CVPD) who is analyzing factors that influence whether or not someone gets their second dose of the mpox vaccine in Ontario.
The 2022 mpox outbreak
Mpox is endemic in certain regions of western Africa, but in early 2022, there was a global outbreak of mpox. At that time, there were an estimated 1,500 mpox cases in Canada, concentrated in Ontario, Quebec and British Columbia. The virus primarily spread through sexual or close contact. Men between the ages of 18 and 49 who have sex with men were disproportionately affected.
To better understand mpox experiences and perspectives from this population, Associate Professors Darrell Tan and Daniel Grace are conducting a series of in-depth interviews with participants from across Canada. Speaking with more than 50 gay, bisexual and queer men, they’ve heard how the 2022 mpox outbreak was reminiscent of the HIV epidemic.
“The legacy of the HIV response and institutional homophobia led many participants to have a lack of trust in public health institutions,” says Grace, whose project is funded by a Canadian Institutes of Health Research grant. “Across Canada, 2S/LGBTQ+ community organizations, many that were founded in response to the HIV epidemic, worked with public health to create safe spaces for gay, bisexual and queer men to be vaccinated and seek resources for mpox.”
Since the 2022 outbreak, mpox case counts have been on the decline — until this year.
Certain regions in Canada have seen a rise in mpox cases this year, according to the Public Health Agency of Canada (PHAC). For instance, Ontario has already seen more than six times the number of confirmed cases (206) compared to all of 2023 (33 confirmed cases). The increased number of cases prompted public health experts to renew calls for vaccination.
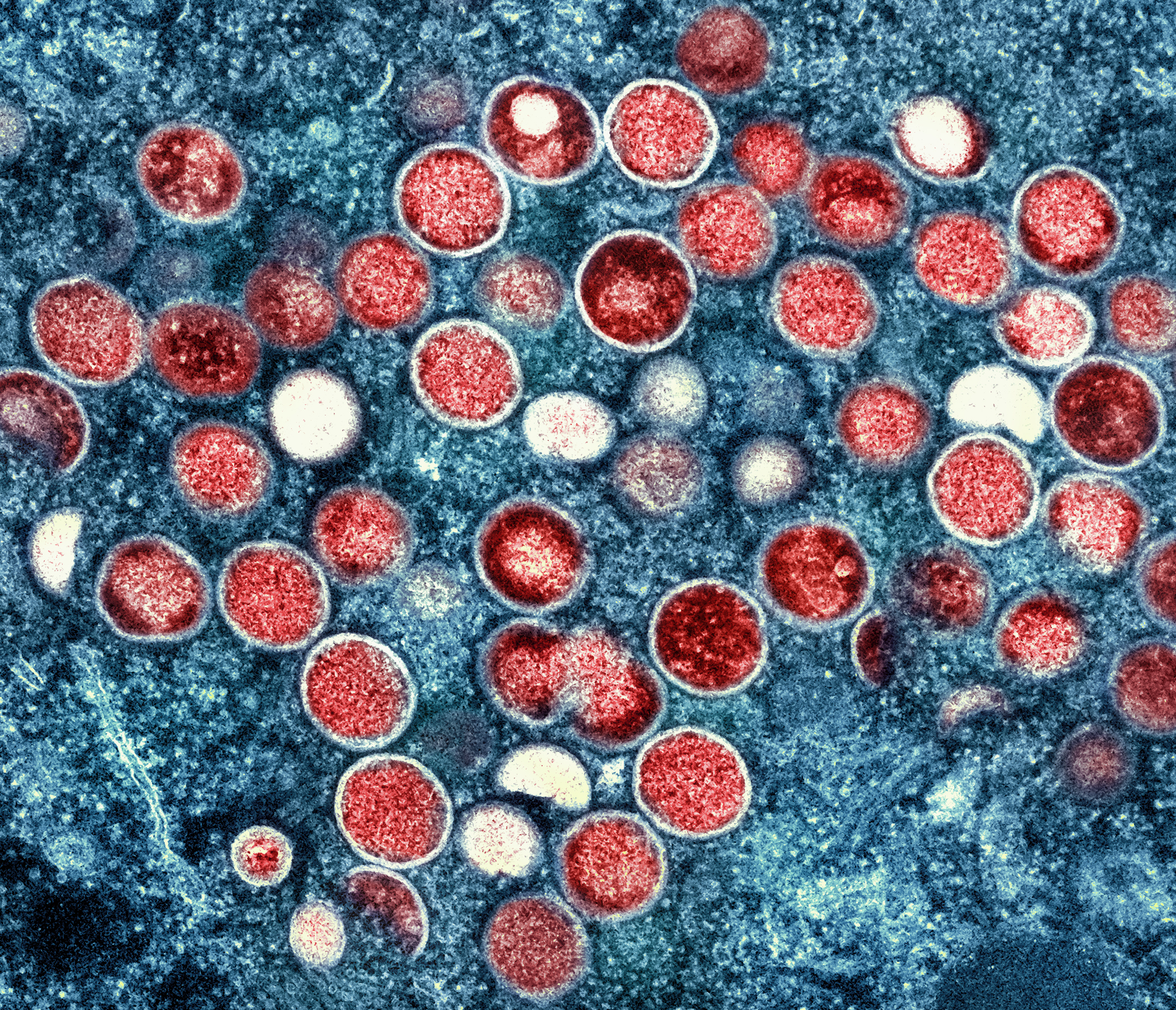
Mpox particles (red) found within an infected cell (blue), cultured in the laboratory. Image captured and color-enhanced at the NIAID Integrated Research Facility (IRF) in Fort Detrick, Maryland. (Photo: NIAID)
Mpox vaccination and eligibility
In Canada, the vaccine used to protect against mpox is called Imvamune. This vaccine is currently only offered to individuals who are at high risk of being exposed to mpox, such as sex workers and gay, bisexual, or other men who have sex with men. Imvamune was initially authorized for use in Canada in 2013 for smallpox, which has similarities to mpox, and was found to be effective against mpox as well.
“The vaccine works by training your immune system to fight off mpox if you are later exposed to it,” explains Grewal. The vaccine has also been shown to reduce how sick individuals get if they do contract mpox and the likelihood of ending up in the hospital. She adds that Imvamune “does not contain smallpox or mpox and cannot spread or cause these infections either.”
With the increase in cases, public health experts are encouraging those eligible to get two doses of the available vaccine.
Studies from the U.S. show that two doses — which is considered being fully vaccinated against mpox — offers better protection against mpox than one dose.
The National Advisory Committee on Immunization (NACI) recommends that individuals at risk of contracting mpox receive two doses of Imvamune, at least 28 days apart. This is also the official public health recommendation in Ontario. However, out of all the individuals in Ontario who received one dose of Imvamune, only 37 percent have received a second dose, according to PHO.
“As we learn more about mpox, it’s clear that one dose offers some protection but it’s crucial to get a second dose to be as protected as possible,” says Grewal. “If you are eligible, you can go to your local public health clinic(s) to receive your second (or first) dose. You can also inquire about vaccine availability where you access sexual healthcare services.”
Community organizations and mpox vaccine access

Associate Professor Daniel Grace
Through their ongoing research, Grace and his team are hearing how important community-based organizations are to mpox prevention. Vaccine drives and promotional efforts from local organizations like Toronto’s 519 and AIDS Committee of Toronto (ACT) were key to vaccine uptake in 2022, says Grace, “and remain vital to the ongoing mpox response.” However, Grace and colleagues are hearing that this year, access to mpox vaccines is challenging and many participants are uncertain about when or if they needed a second dose.
“In Toronto, we learned from many people that there was a lack of availability of mpox vaccines this year, forcing those seeking vaccines to head to the outskirts of the city to receive first and second doses. It is necessary to consider the vaccine equity issues here, including those who are not able to travel to access vaccination,” says Grace, who is also a CVPD member. Community organizations like the Gay Men’s Sexual Health Alliance and the Community-Based Research Centre have put together mpox information to help address misconceptions and improve access to vaccination.
“The more places vaccine access can be integrated into people’s regular sexual health routine, the better,” says Grace.

Assistant Professor Ramandip Grewal
Mpox in the Democratic Republic of the Congo — and why it matters here
In addition to mpox in Canada, public health officials are keeping an eye on the rising number of cases around the world. More than 120 countries have confirmed cases of mpox since the onset of the global outbreak in 2022.
The Democratic Republic of the Congo (DRC) has been hit particularly hard by the virus, reporting more than 8,000 cases, including 25 deaths so far this year. Experts are particularly concerned given the humanitarian crisis in DRC and the risk of mpox spreading in overcrowded camps housing millions of displaced people.
The WHO also recently warned that the DRC is experiencing cases of a new variant of mpox. Person-to-person spread of this variant also occurs through close contact and is impacting larger populations including women and children.
“Though we haven’t seen this variant of the virus in Canada yet, there is always a possibility that it could spread here through travel,” says Grewal. “The risk of that is suspected to be low to moderate at this time. Nonetheless, it’s another reason why it is important for those eligible to go get vaccinated.”